Your period changes as you age. Learning about why certain changes happen will help you prepare to deal with them.

A woman’s body is constantly going through changes. Lucky for us, we get a front row seat reminder of those changes every month. And as we get older, it may seem like we know everything about how our body changes during our periods. Especially since we’ve been having one each month starting in our teens. But the truth is, we may not know everything because our period changes as we age.
It’s true. Your age can have a major impact on your menstrual cycle – how long your periods last and even how heavy your flow will be. This is thanks, in part, to normal age-related hormonal changes.
Sometimes your period changes so much so that you may not even know what to expect. Which can be a pain to deal with.
Read on to find out how your period changes as you age starting from your teens and into your 20s, 30s, 40s, and 50s and beyond.
Your Period
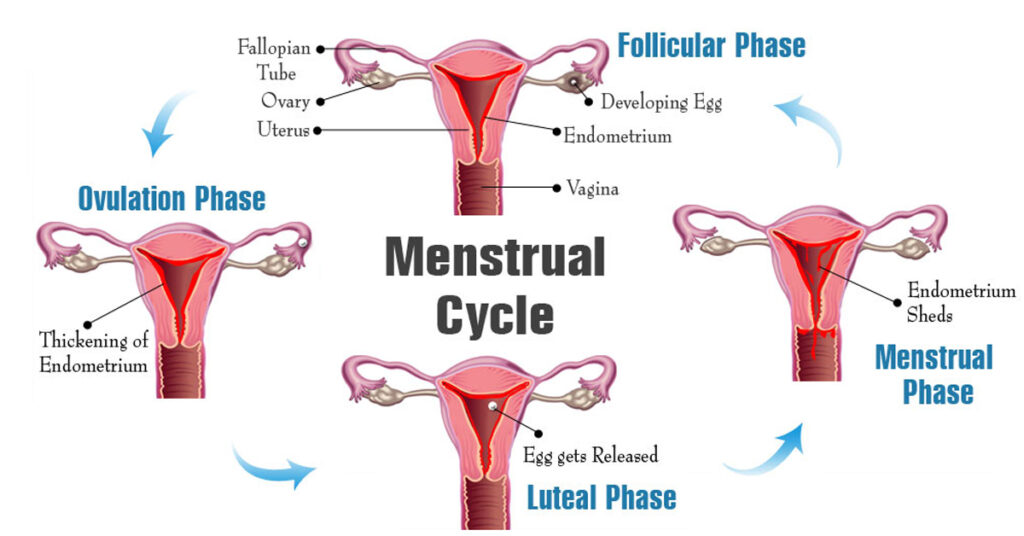
A period refers, specifically, to the stretch of time where you are actually bleeding. On more technical terms, your period is the part of your menstrual cycle when the uterus sheds its lining.

Your Menstrual Cycle
It is common that people use the term menstrual cycle interchangeably with period. However, your menstrual cycle doesn’t just refer to your period. It’s the whole gamut of events starting with the first day you get your period. And it includes the time your ovaries release an egg (ovulation) through to your uterus lining thickening in case that egg gets fertilized – meaning you get pregnant. And then to the shedding of that lining (your period) if you are not pregnant.
Your entire menstrual cycle can go from 21 days to more than 35 days. Your cycle will not always be the same – it can change from one month to the next. And your periods can be completely different from even your mom and sister.
What Is A “Normal” Period?
I’m going to go out on a limb and guess that your period is probably not your favourite monthly event. Especially when your period doesn’t go exactly as expected. It’s late one month and early the next. Your flow can be light for several months, then all of a sudden, it’s heavy and lasting the entire week. That’s not it – there’s the premenstrual symptoms (PMS), such as moodiness, irritability, etc., – and cramps that can knock you out one month but not even make a peep the next.
Those monthly changes can also come in the form of hormones fluctuations, breast tenderness, and sometimes even a bit of acne on your face. It’s just part life for many years for most women.
As unpleasant as these unpredictable changes may be, that is how it is as you get older.
Because your periods will keep adjusting and evolving month to month due to age-related hormonal changes. And your hormones dictate every aspect of your menstrual cycle and periods.
Since your hormones fluctuate during different stages of your life, it makes perfect sense that your periods would change too.
Factors That Can Impact Your Period
However, there are other factors that can have a major impact on how your period changes at any age. Factors such as stress, diet, lifestyle, whether you are using contraceptives, the type of contraceptive you are using, whether you have had a child, your fertility, medications you are taking, certain medical conditions you may have, and even your genetics.
Needless to say, no menstrual cycle and period are the same. And there’s no such thing as a “normal” period because each woman is so different. Normal is different for every woman.
With that said, however, there are some typically accepted characteristics of a healthy monthly period. So, what is “normal” and what should you be concerned about?
Learning about what these changes are and why they are happening will help you prepare for them.
In Your Tweens or Teens
This was a shocking statistic to me – turns out, the average North American girl gets her first period at around 12 years old. Some may get it a few years older or younger – and that’s normal too.
The age in which you get your first period can be influenced by your genetics, how much baby fat you still have on your body (your Body Mass Index, BMI), the foods you eat, and how much exercise you get.

For the first couple of years you get your period in your tweens and teens, it is common for it to be irregular and unpredictable. You might go months without having one after your first period. And then seemingly out of nowhere, boom – it can return with a vengeance. Your period can be 3 days or it can last up to 7 to 10 days. What is predictable about your period at this age is that it is very unpredictable. And that is perfectly normal for it to be so at this age.
This is because at the beginning when you first start getting your period, you may not be ovulating. As I mentioned, your reproductive hormones, estrogen and progesterone, controls your menstrual cycles and your periods.
And at this age, your body may not have the amount of hormones to stimulate and regulate ovulation consistently yet. And so, your period at this age can be very erratic. It can come or not come every month and it can be heavy or light.
With that said, however, if you find that your period starts becoming really irregular or stops altogether, it may be worth speaking to your doctor or gynecologist. That is not to say that there is anything wrong per se, but more to rule out things, like Polycystic Ovarian Syndrome (PCOS).
In Your 20s
If you were trying to figure out your period in your teens to no avail, rest assured that your period in your 20s will become more consistent. Meaning that one of the major changes in your 20s is that your period starts to settle into a regular rhythm arriving monthly. It can be so consistent that your periods may be the same length of days and also, the same heavy or light flow each month.
Essentially, your menstrual cycle and period become more predictable at this age. So, no more worrying about any surprise appearances at the worst times.
In fact, for some women in their 20s, their cycles will be the most regular. That is because this is the time your body is most prepared to have a baby.
The reason has to do with the change in the amount of hormones coursing through your body at this age. Which, in turn, causes you start ovulating more regularly and thus, have more consistent periods in your 20s. This also means that you may also experience more period-related symptoms more regularly. Symptoms such as PMS, abdominal pain and cramps, and breast tenderness. To alleviate some of those symptoms, many health care professionals will offer some form of contraceptives to help.
That is not to say that contraceptives are the only way to ease period pain and cramps. Your lifestyle and diet can have a major impact on the severity of your period-related symptoms. But unfortunately, contraceptives are the most commonly used by doctors. Therefore, it is prudent to discuss contraceptives in relation to its impact on your periods.
Contraceptives Can Change Your Periods
Another major change that can affect your menstrual cycle and tends to happen in your 20s is the use of contraceptives. That is, this is the time when most young women begin to consider starting on birth control pills or other contraceptives (e.g. intrauterine device, IUD).
Now, depending on the type, some contraception options may change your periods by making them shorter in duration, lighter in flow, and more regular with less bleeding, and less pain and cramping. And some may reduce your PMS symptoms on a whole, while others may even cause your periods to disappear.
Types of Contraceptives
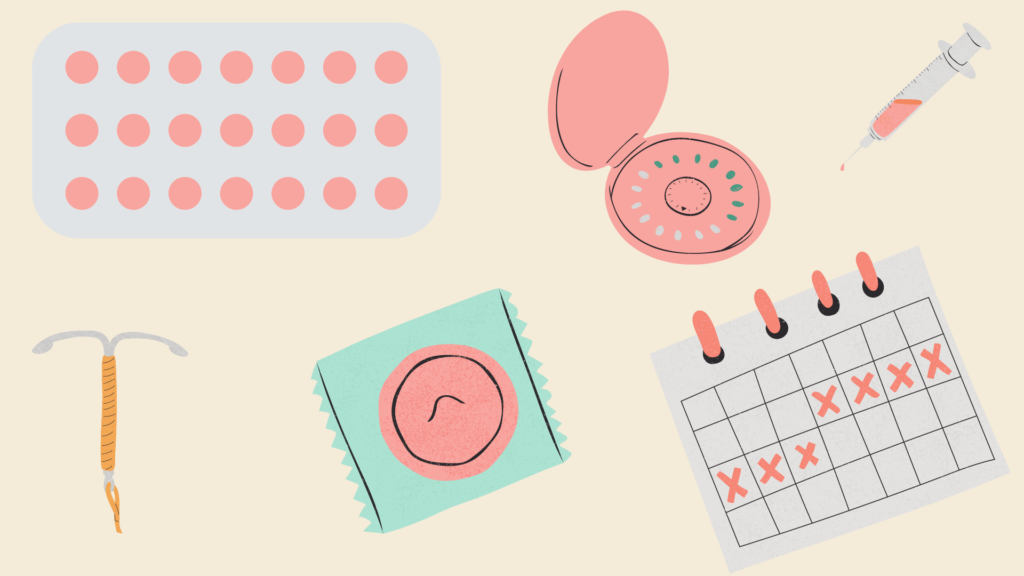
- Non-hormonal Intrauterine Device (e.g. Copper IUD) is a small T-shaped device that is inserted inside your uterus. It works by blocking the sperm’s path into your uterus to prevent fertilization of the egg. This can lead to bleeding in between your periods.
- Hormonal IUDs (e.g. Mirena) secrete a tiny amount of progesterone inside the uterine cavity. This causes a thickening of your cervical mucus, which blocks and traps sperm from fertilizing an egg. This can lead to lighter and less painful periods. However, sometimes it can completely block your periods so you don’t have your monthly period.
- Birth control pills or oral contraceptives contain synthetic hormones that mimic your own reproductive hormones, like estrogen and progesterone. Some pills (combination pill) work by preventing your body from ovulating. Meaning you ovaries won’t release an egg; thus, no period. While other pills (progestin-only pill) cause your body to thicken your cervical mucus to prevent sperm from reaching the uterus to fertilize the egg. Birth control pills are typically prescribed to help regulate your period or to help alleviate painful periods. It can result in shorter, lighter periods with less cramping.
- Birth control injection (e.g. Depo-Provera) contains the synthetic hormone, Progestin. This is similar in structure to your natural hormone, progesterone. It prevents ovulation and when you don’t ovulate, your uterine lining does not thicken. As a result of no thickening of your uterine lining, there is no shedding. Thus, no period. Because you get a birth control shot every 12 weeks, you don’t have a period every month. Rather, you only get your period in between your shots – so, that is, you have a period only 3 to 4 times per year. When you do get your period, it will most likely be shorter and lighter with minimal cramping.
There are many other types of female contraceptives. These are only the more commonly used ones that can affect your menstrual cycle and periods.
Contraceptives Are Not ‘One-Size-Fits-All’
It is important to note that different hormonal contraception will impact your menstrual cycle and period differently. There is no ‘one-size-fits-all’.
Therefore, there may be a trial-and-error period before you settle on one that is right for you. Also, another thing to note is that with every type of contraceptive you will experience some sort of side effects.
In Your 30s
Like in your 20s, your menstrual cycle in your 30s should still be quite predictable and consistent. For most women, however, a huge game-changer to your period is pregnancy. Of course, getting pregnant can happen anytime once you start your period. But over the past few decades, more and more women are waiting until they are in their 30s to start having babies.

We all know that getting pregnant means you don’t have a period for the entire time of your pregnancy. And your period doesn’t usually return until about six weeks after you deliver your baby if you are not breastfeeding. However, if you are breastfeeding, your period usually will not return until you stop nursing or even a year after that.
In addition to the changes during and immediately after your pregnancy, having a baby can lead to long-term changes to your menstrual cycle. For some women, when their period returns after pregnancy, they will have lighter and shorter periods, and their period cramps may get better. This can be because their cervical opening becomes a little bit bigger after vaginal delivery. Thus, their flow comes without needing a strong uterine contraction. However, for other women, they may experience heavier, longer or more painful periods after having a baby.
Period Changes In Your 20s and 30s You Should NOT Ignore

As mentioned, your menstrual cycle is usually the most stable in your 20s. But there are changes to your period that may be a sign of a menstrual condition. Here are some conditions that can change your period:
- Polycystic ovary syndrome (PCOS) – Discussed in a previous post (read it here), PCOS is a condition where you produce higher-than-normal amounts of male hormones. As a result of this hormone imbalance, your body may skip your monthly period.
- Endometriosis – This is a condition in which tissue that is similar to the tissue that lines inside your uterus grows outside your uterus. This tissue is called endometrial tissue. This can cause painful periods, prolonged cramping, and heavy period bleeding or bleeding between your periods.
- Endometrial Polyps – These are abnormal growths inside your uterus or on your cervix. Polyps are made up of the same tissue that makes up your uterus lining, endometrial tissue. Most of the time, endometrial polyps are benign (non-cancerous); however, they do have the potential of becoming cancerous. This can cause irregular periods, bleeding between periods, and very heavy period bleeding.
- Uterine Fibroids – Like polyps, these are also abnormal non-cancerous (benign) tumour growths that develop on the outside or inside the wall of your uterus. Unlike polyps, they are rarely cancerous. Another difference is the tissue they are made of. Fibroids are made up of connective fibrous tissue. This abnormal growth can cause heavy bleeding between or during your periods that can include blood blots, periods lasting longer than 7 days, painful periods, and severe menstrual cramping.
Because your periods in your 20s and 30s are typically more stable and regular, it will be easier to spot abnormal changes to your periods.
If you experience a super heavy period flow, abnormally long periods, debilitating period pain, or bleeding between your periods, do not hesitate to see your doctor.
In Your 40s
Your 40s mark the beginning of a brand-new hormonal journey: perimenopause. Perimenopause is defined as the span of years – 8 to 10 years – before menopause. And it is the result of your body starting to produce less estrogen and progesterone to prepare for the menstruation finish line, menopause. This typically happens in your early 50s.

During perimenopause in your 40s, normal fluctuations in estrogen levels will cause ovulation to be more irregular. Which means you could start experiencing major changes to your menstrual cycle like you did in your 20s. Changes such as missed periods, a heavier flow, spotting between periods, and even longer than usual PMS and cramping. And like your period in your 20s, what is predictable about perimenopausal symptoms is that nothing is predicable.
Your Irregular Periods May NOT Be A Perimenopause Symptom
One thing to keep in mind is that irregular periods in your 40s are not enough to say for certain that you are experiencing perimenopause. Because perimenopause usually comes with other corresponding signs and symptoms, such as:
- Hot flashes
- Chills and night sweats
- Trouble sleeping soundly
- Mood swings and emotional ups and downs
- Weight gain
- Drier-than-normal vagina
- Thinning hair and dry skin
- Loss of breast fullness
But if you don’t notice any of these accompanying perimenopausal symptoms with your irregular periods, it may be prudent to go see your doctor.
In Your 50s And Beyond
Your 50s kickstart the beginning of the end of your menstrual cycle – menopause. You are officially in menopause when you haven’t had a period for 12 consecutive months. And the average age a woman goes through menopause is 51 years of old. But there are factors that can influence the age at which you start menopause. Factors such as the number of babies you have had (more babies can mean later menopause), if you are a smoker you may have menopause 1 to 2 years earlier. And your ethnicity can impact your age of menopause. For example, African American/Canadian and Hispanic women tend to have earlier menopause than Caucasian and Asian women.

The good news about menopause is that you can expect your perimenopausal symptoms to ease quite a bit. But they won’t all completely disappear because your ovaries will continue to cause some hormone activity. So, for some, you may still experience monthly moodiness and irritability. And it can even be an emotional roller coaster for you during menopause. But that is completely normal.
The Bottom Line
As discussed in a previous post, a woman’s body is amazing! Because whatever your age, your body offers a lot of insight into your overall health. Although your period changes as you age, it is still a good indicator of what may be going on in your body.
Your period will change as you age, but some changes may not be normal age-related changes. So, pay attention to what is normal for you. Because every woman is different and a normal period is different for every woman.
Knowing what your normal looks like will help you identify any unusual symptoms or sudden changes in your menstrual cycle.
Basically, your menstrual journey is like a bloody snowflake. Every one of your periods is unique!





