7 Thing To Do To Shape Your Baby’s Gut Health

From the very moment your baby is born, it sets off a complete transformation of your baby’s gut. The biggest change is the introduction of microorganisms, which includes bacteria, viruses, archaea, and fungi – to form your baby’s gut microbiome. (I discussed the gut microbiome in detail in a previous post; you can read it here.)
And interestingly, your baby’s gut microbiota can shape her health in later life. It’s true. These tiny but powerful microorganisms can either help prevent or lead to disease in later life.
That is why we have been hearing so much about the gut microbiota in more recent years. So much so that many of us believe that a healthy gut microbiota may be the treatment or even cure for many diseases from asthma to allergies to obesity.
Unfortunately, it may not for you. You already have an established microbiome.
For your baby, however, now that’s a different story!
Although certain things that happen during delivery are oftentimes outside of your control, there are other ways you can help nourish your baby’s gut health that are safe and beneficial.
Before I dive deeper in ways you can shape your baby’s microbiome, I want to give you some context in terms of my background in this area of research.

As I mentioned in Part I of this Microbiome Gut Health series (read it here), during my post-doctoral fellowship, I designed and conducted a clinical trial called the ProGut Study. The aim of the study was to investigate how a baby’s microbiome develops and the factors that affect its development. I examined how the use of probiotics and antibiotics during early childhood can change the type of microbes that live in a baby’s gut microbiota. Also, how that affects a child’s overall health in later life.
So to say this is a topic I studied is hugely understating my genuine interest on this topic.
Your Baby’s Gut Microbiota
So, how do babies acquire their gut microbiota?
Babies are born sterile – meaning they enter the world with essentially no microbes in or on their tiny bodies. However, as I mentioned in my previous post, there have been some debate whether in fact babies are sterile in the womb. Nevertheless, the widespread understanding is that babies start to receive their first microbes when they are born. From either their mamas, as they travel down the birth canal, or from the environment of their birth if they were delivered by C-section. In the first few days of a baby’s life, there is even more transmission from mama – something as simple as physical contact can transfer mama’s good bugs to baby.
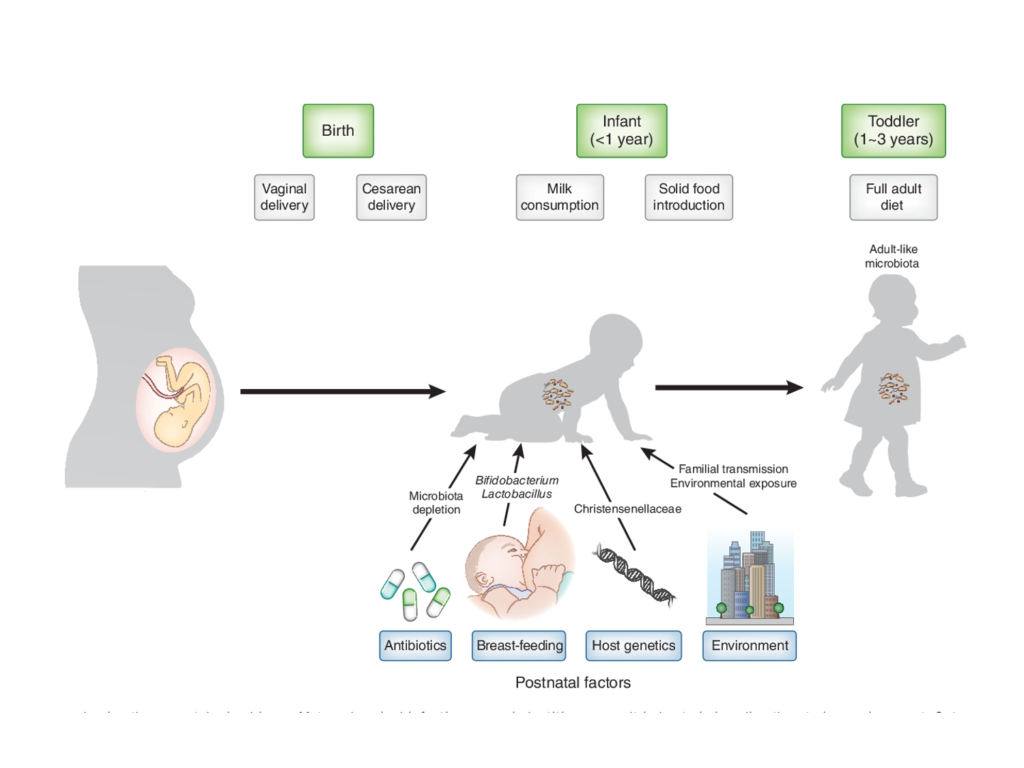
As baby grows and matures, so does her gut microbiota until about 3 years of age. At which point, her bacterial communities more resemble that of an adult’s gut microbiota. Meaning that as it becomes more adult-like, it gets more diverse and more resilient to change. But that doesn’t mean that your baby’s gut microbiota stops maturing at 3 years of age. In fact, changes in the species and strains of bacteria can be seen even up to 20 years of age. And even more shifting of bacterial communities happens at about 70 years of age into the elderly type.
Despite that, from birth to about 3 years of age is a critical stage of your baby’s gut microbiota development. This emphasizes the importance of nurturing your baby’s gut bacteria to keep her gut microbiota growing healthily.
Why it is important to have a healthy gut microbiota at an early age?
Well, a baby’s gut microbiota and immune system actually develop together – essentially teaching and learning from each other.
In other words, the first microbes that makes its way to a baby’s gut – also, on her skin, mouth, and nose – help teach her immune system to distinguish between the friendly versus harmful bacteria. And so, when there is a disruption in the seeding of the first microbes, it leads to an improperly developed immune system. This may lay the foundation for a greater risk of developing health problems.
During my fellowship training, my group and I found that a baby’s microbiota is quite unstable, dynamic, and more impressionable than that of an adult. And more, we learned that certain changes to the gut microbiota during infancy may affect their risk for certain diseases. Diseases such as asthmas, allergies, obesity, and even autoimmune diseases.
Basically, what this all means is that there are factors that can impact the development of your baby’s microbiome, which can shape her health in later life.
Your Baby’s Microbiome Can Shape Her Health Later Life
Now, most mamas know that even the best pregnancy and birthing plan may not turn out as expected. And that is perfectly okay because some things are just simply out of our control.
With that said, however, there are other things that we can do to help nourish our baby’s gut health that are safe and may be of some benefit.
1. Eat a nutrient-dense, fibre-rich whole food diet while pregnant and breastfeeding.

A major function of your gut microbiota is to digest, extract, and produce energy for your body from the foods you eat. And so, eating a high fibre whole food diet during pregnancy feeds and nourishes the ‘friendly’ bacteria in your gut.
Additionally, high fibre diets allow the friendly bacteria to produce short-chain fatty acids (aka. ‘gut food’) as a byproduct of fibre metabolism. Now, short-chain fatty acids (SCFAs) play an important role in health and disease. They are essentially the main source of nutrition for the cells in your colon. More specifically, acetate and butyrate are 2 SCFAs that are involved in strengthening your gut lining and, in turn, support your immune system. As a result, these SCFAs may help lower the risk of autoimmune diseases.
I literally could go on and on about SCFAs and its role in our gut health, but that will have to be another post.
It is also very important to eat a wide variety of fibre-rich, nutrient-dense foods to ensure that there is food for every type of bacteria. This increases the overall diversity of your gut bacteria. Which, in turn, builds a community of good bacteria that you can pass along to your baby during delivery, through your breast milk, and even with skin-to-skin contact.
And so, it is not only about what to feed your baby, but also what you feed yourself. Because the health of your gut microbiota helps shape your baby’s gut microbiota.
2. Try to reduce your risk of a C-section and opt for vaginal delivery, if possible.
First, a C-section is a life-saving medical intervention. Especially in emergencies situations, it can be a matter of survival for both mama and baby. So, I am the first to say how amazingly grateful I am to have this medical option available to those who need it. Without them, my husband and brothers would not even be with us.
With that said, more recently, research has shown that delivery by C-section may alter the initial bacteria that are seeded in a baby’s gut microbiota. This is because of the first microbes a baby encounters when delivered by C-section comes from the doctors, nurses, and delivery suite she was born in. In contrast, vaginally delivered babies begin collecting mama’s microbes as she travels down the birth canal. Thus, emerging into the world covered head to toe in mama’s good bacteria. This difference may have a profound effect on the development of baby’s gut microbiota.
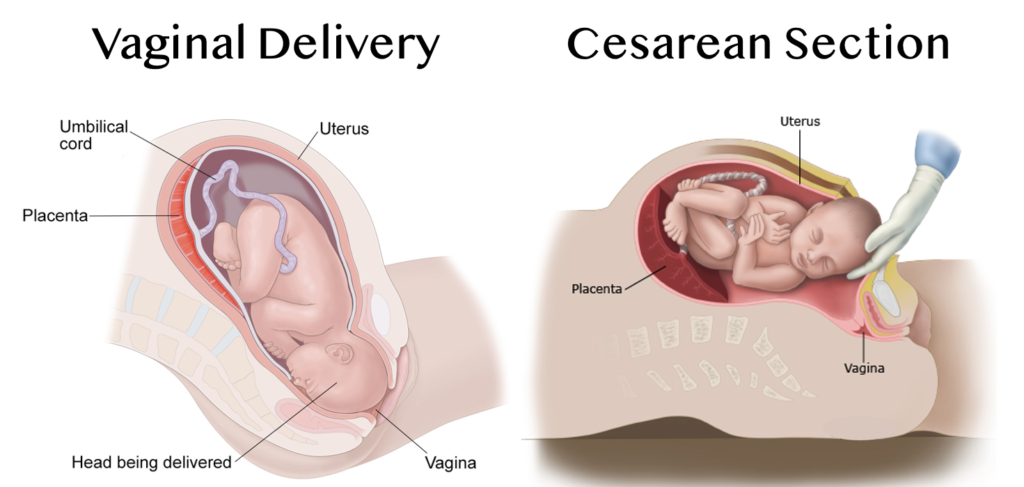
Image may be subject to copyright.
The type of bacterial communities that a baby initially encounters may take months, if not years, to see its effects. Though it may not be permanent, some researchers have suggested that this difference may have health implications for the baby in later life. For example, there is some evidence indicating that some babies born via C-sections are at higher risk for obesity, allergies, asthma. However, more research is needed to conclusively determine this link.
3. Give ‘em some skin. Skin-to-skin contact with baby as soon as possible.
Again, birth is unpredictable, and C-sections should not be avoided when it is deemed necessary. Because fortunately, no matter how a baby is delivered, there are other steps moms, and let’s not forget dads, can take to ensure baby’s bacterial communities gets off to a good start. And it is with immediate skin-to-skin contact with baby.

Lots of skin-to-skin contact between mama and baby immediately after birth can help seed newborns with mama’s good bacteria. This was discovered in a study where researchers looked at two group of premature babies: one group were held briefly skin-to-skin by their mamas and the other group mama’s were unable to do so. They found that preemies with skin-to-skin contact had mouth and gut microbiotas that resembled some of mama’s bacterial colonies. And this group of preemies had a greater immune tolerance and were slightly more protected against infections. Infections such as necrotizing enterocolitis (NEC), a condition that affects preterm babies’ intestines. Whereas preemies with no skin-to-skin did not have any of mama’s bacteria on them and had a higher incidence of developing NEC.
But don’t stop skin-to-skin with your baby after just a few days. Studies found that transfer of mom’s good bacteria happens up to 3 months. At which point babies’ gut bacteria start to resemble that of her environment and other people she is exposed to. Oh, and don’t feel left out dad because skin-to-skin with your baby transfers your good microbes too. It also helps start building that baby and daddy bond. So, strip down and give your baby some skin!
4. Don’t be so quick to throw your baby in the bath tub with the bath water!
You may have noticed that after delivering your baby, the nurse handed you your precious bundle wiped down and swaddled up. Perfectly clean she may not be, but that is how you should keep her for at least 24 hours. That is because she is coated in your precious good bacteria and the white substance, called vernix. And so, bathing your newborn could interfere with early bacterial seeding from mama. Also, it will wash away the vernix, which contains proteins that prevent common bacterial infections.

Bacteria and vernix health benefits aside, wouldn’t you want that delightful newborn smell to linger for days? So, consider not bathing your newborn!
5. Have your baby drink any amount of breastmilk possible. Even a little bit is good enough.
The ‘Breast is Best’ public health campaign – although given with good intentions – is stress-inducing for some mamas, myself included. This campaign, echoed by many OB/GYNs, family care physicians, and midwives, encourages mamas to exclusively feed their babies breastmilk for the first six months. But for some mamas, at no fault of her own, are unable to follow this guidance exactly as directed. And that is okay. Actually, more than okay.
Because, in my opinion, whether it is formula or breastmilk – ‘fed is best’.
Interestingly, more recent research discovered the ‘breast is best’ campaign is given not so much for the long-term health benefits of your baby. But rather, breastmilk is more beneficial for your baby’s gut bacteria than your baby herself. Let me explain.
Here’s some circular logic for you: so, human breastmilk contains a component called human milk oligosaccharides (HMOs). HMOs are essentially complex sugars with distinct bonds and these HMOs are the third largest component in breastmilk. Even though HMOs are abundant in breastmilk, HMO bonds cannot be broken down by your baby’s digestive enzymes. Meaning, your baby cannot digest them. And that’s the kicker – why would mamas go through so much effort to produce these HMO sugars when babies cannot extract the energy from them?
In fact, HMOs simply bypass your baby’s stomach to get to her colon, where all her gut bacteria exist. What researchers have discovered is that HMOs are actually mama’s fibre, a prebiotic. They are essentially food for the bacteria in your baby’s gut. In particular, HMOs feed a specific species of bacteria, Bifidobacterium. Bifidobacteria actually contain specific genes that break down the HMO bonds so they can feed off of it.
Why is it important to nourish your baby’s gut bacteria with breastmilk?

Well, much of our immune system is in the lining of our gut, which helps keep ‘bad’ bacteria and viruses out. The cells on the gut wall are responsible for absorbing nutrients from our food, thus, nourishing the ‘good’ bacteria present there. This, in turn, strengthens our immune system.
Because babies are born with a very immature immune system, nurturing your newborn’s gut bacteria with HMOs essentially contributes to the development of a strong immune system. Studies have shown that early seeding of good bacteria in your baby’s gut microbiota leads to early development of her immune system. And both developing together lowers the risk of developing food allergies, childhood asthma, and obesity.
But, what about babies who are not getting breastmilk? Or, like some babies, getting a combination of both breastmilk and formula? In other words, how does formula affect the gut microbiota?
Well, studies have shown that exclusively breastfed babies do have gut bacteria that differs from those who are exclusively formula fed. Breastfed babies have more diverse species in their gut microbiota. And because HMOs selectively promotes the growth of this particular species, breastfed babies tend to have more Bifidobacteria than formula fed babies.
But that is not to say that formula fed babies are at a huge disadvantage. At least, not anymore. That is because many formula manufacturing companies now add prebiotics and probiotics to their infant formulas. This is done in attempt to mimic components in breastmilk. Therefore, more recent data show that babies fed pre- and pro-biotic supplemented formulas have gut bacteria that more closely resembles that of exclusively breastfed babies.
More research is needed to figure out whether these supplemented formulas provide any long-term health benefits for baby.
Going back to the ‘breast is best’ campaign, it would be more accurate to say: ‘breastmilk is best for baby’s gut bugs’. For baby though, ‘healthy bugs are best’. And it does not matter where these bugs come from as along as they get there!
6. Avoid any unnecessary use of antibiotics

Like C-sections, antibiotics are life-saving. If you have a bacterial infection, there is no doubt you need them. So, I am not debating its usefulness.
Antibiotics work by eliminating bacteria responsible for infections. But in doing so, the unintended consequence is also getting rid of the ‘good’ bacteria, which may negatively influence overall health.
More worrisome is that antibiotics are among the most over prescribed drugs in kids. They are often given for mild illnesses that would probably resolve on its own. And worse, they are even prescribed for viral illnesses, such as the common cold and ear infections, for which antibiotics are completely ineffective.
The concern with over-prescribing antibiotics to kids is not just the unintended consequences of causing certain strains of bacteria to become resistant (antibiotic resistance bacteria). But also because antibiotics wreak havoc on their underdeveloped gut microbiota. One course of antibiotics can decimate multiple species of friendly bacteria. Thus, lowering the diversity of bacteria in your baby’s gut microbiota.
More than that, my group and I published a study showing that this disruption may contribute to later life diseases, such as asthma, allergies, IBD, and obesity. The evidence also indicates that these risks appear greatest for young children exposed to antibiotics in early life.
How to prevent overuse of antibiotics?
I want to stress that I am not against the use of antibiotics when it is necessary. Because, in some instances, antibiotics are truly necessary. I am advocating for more judicious use of antibiotics.
And so, when your baby gets a prescription for antibiotics, I recommend double checking with your doctor or pharmacist whether it is, in fact, necessary. Before rushing to fill the prescription, ask if it is possible that your baby’s infection would resolve on its own. Because, sometimes, doctors feel parental pressure to prescribe something, as some parents feel something is better than nothing. In the case of antibiotics, however, oftentimes nothing is better than something when it comes to the sniffles or viral infections.
And lastly, opt for using plain old soap and water instead of antibacterial soaps or cleaning products. Because these products may also disrupt your baby’s developing gut microbiota by killing off not just the bad bugs, but also, the good and necessary bugs.
7. When antibiotics are absolutely necessary, give probiotics to help lessen the side effects.
Ahh, probiotics. Not only are they the most talked about supplement in recent years. But also, the one ingredient that seems to be added into everything. From yogurt to frozen treats to granola bars to even baby’s body wash and skin care products. In some products, it is a bit gimmicky, but it sells because it is touted to improve gut health.
So, the question is: does giving your baby probiotics help improve her gut bugs?
The answer in some cases, it is a resounding YES!

Image may be subject to copyright.
For instance, if your baby required a course of antibiotics, giving your baby probiotics during and/or after that course has been shown to cut their risk of antibiotic-associated diarrhea in half. Also, probiotics may also help replenish the good bacteria lost due to the antibiotics. The best time to give it is between antibiotics doses to prevent killing off the live bacteria in the probiotics
My PhD work looked at using probiotics to treat infant conditions, such as infantile colic. And so, giving your baby a specific strain of probiotic, Lactobacillus reuteri, significantly reduces newborn colic. For other conditions, such childhood eczema, probiotics has also been shown to reduce the risk of flare ups.
And probably the most effective use of probiotics is for preemies. Probiotics have been repeatedly shown to be effective at cutting the risk of necrotizing enterocolitis – a severe and often fatal condition – in half.
The evidence indicates that a probiotic cocktail, meaning a mix of multiple bacterial strains consisting of Lactobacillus and Bifidobacteria, appear to be most effective for the childhood conditions mentioned.
Current Clinical Studies on Probiotics for Babies
Now, many have asked whether probiotics can be used preemptively to prevent conditions. Conditions such as infantile colic, allergies, asthma, and baby eczema. The answer to that is: we are currently investigating this. In fact, I am a co-investigator on a study conducted at SickKids Hospital in Toronto, Canada where we are giving newborn infants a probiotic in the first few days of life. Essentially ‘seeding’ a baby’s gut microbiota with a probiotic to see if infantile colic can be prevented. The study is currently ongoing, so, stay tuned.

Image may be subject to copy right.
Lastly, when adults take probiotics, its effects are temporary. Meaning that the probiotic will help alleviate gut symptoms for the time they are taking them. This is because adults have an established gut microbiota.
Unlike adults, however, babies’ gut microbiota is more unstable and more impressionable because their microbiota is not fully developed yet. And so, the idea of giving a baby a cocktail of ‘friendly beneficial’ probiotics to see if it would help seed their gut microbiota is a question I sought to answer.
Therefore, during my post-doctoral fellowship at McMaster University in Hamilton, Canada, I designed and conducted a clinical trial to answer this specific question. We found that giving kids younger than 3 years of age a probiotic temporary changed the bacterial community in their gut microbiota.
In other words, probiotic use in kids may be more effective at shifting the type of bacteria in their gut microbiota than in adults. Whether the probiotic’s beneficial health effects are long lasting is not yet known. Thus, more research is needed.
The Bottom Line
Of course, all mamas want to set our baby’s health off to a good start. And yes, keeping their gut microbiota healthy is a way to get there. What is important to remember is that there will be situations that arise that will be out of our control. But that does not mean you have doomed your baby’s gut health. All it means is that you can’t do those things you can’t control, but consider doing the other things that you can control. And by taking those steps, you can help boost your baby’s microbiota that way.
Before you know it, your baby will be digging in dirt, mouthing other kids’ toys, and boosting their own microbiomes their own way! So, in the meantime, don’t fret, give your baby a big kiss (to transfer your good mouth bugs) and do what you can because that alone is enough.






Amazing information! Thank you for the eloquent synopsis. Very helpful!
Hi Rachel,
Thank you for your kind words. I am glad that you found it informative. As you can probably tell, I am very interested in the microbiome! So please stay tuned, I will continue this series in the next few weeks.
Thanks again, Rachel!
~Kim